
How three moments of serendipity led to an Alzheimer’s research breakthrough
By Laura Rosbrow-Telem
For more than a decade, biomedical engineering Professors Chris Schaffer and Nozomi Nishimura have studied factors that contribute to Alzheimer’s disease, in the hopes of eventually finding a treatment. Their background in physics enabled them to develop optical tools that allowed them to study Alzheimer’s in new ways, leading to unexpected discoveries. Most recently, their research lab published a paper in Nature Neuroscience that identifies the cause of one major symptom of Alzheimer’s disease – reduced blood flow to the brain – and demonstrates in mice that improving brain blood flow improves memory function.
When Schaffer gives the “elevator pitch” about his work, he usually begins by saying his lab wanted to understand what caused blood flow reductions in Alzheimer’s disease brains. “But to be frank, that’s a lie. That’s not how we came to this, at all,” Schaffer admits.
Only after some serendipity did they come to this part of the puzzle. Now, their research may even lead to a novel Alzheimer’s disease drug target.

The first aha moment
Schaffer reflects that at first, “We were trying to understand the other side of the coin. We were trying to understand how occlusions in blood vessels exacerbate Alzheimer's disease. What we found instead was how Alzheimer's disease leads to dysfunction in the blood vessels of the brain.”
Schaffer and Nishimura’s initial research goal was more basic and not even tied to Alzheimer’s disease. More than 10 years ago, when they both worked in Professor David Kleinfeld’s lab at the University of California, San Diego, Schaffer and Nishimura had developed a laser tool that could induce blood clots, or strokes, in live mouse brains and they wanted to find a good use for it.
At the time, there was a growing body of research that observed a correlation between increased damage to and occlusion of small blood vessels in human brains and the presence and severity of Alzheimer’s disease. For a long time, the most obvious sign of Alzheimer’s disease had been a buildup of amyloid plaques in the brain. But emerging research suggested that patients with the worst symptoms of Alzheimer’s disease had both amyloid plaques and signs of vascular damage; amyloid plaques alone, researchers argued, could not explain the progression of Alzheimer’s disease.
So Schaffer and Nishimura received funding from the National Institutes of Health to apply their unique laser scalpel to induce brain vessel blood clots in Alzheimer’s-affected mice to see if this hastened the disease’s advancement. They were the best suited to lead such research because the most common animal used for Alzheimer’s studies was mice—Alzheimer’s disease mice did not naturally have clots or other damage to brain blood vessels like humans did—and Schaffer and Nishimura were the one of only a couple of labs in the world with a tool that could induce clots in small, targeted brain blood vessels in live mice.
Schaffer says their first big discovery came from one of the undergraduate researchers on their team, Joan Zhou ’08, M.Eng. ‘09. He recalls, “She was doing experiments where she was inducing strokes in the brains of Alzheimer’s mice, and we were looking to see if it made the pathology worse. One day, she came in and was talking about the experiment. She said, ‘Well, I was going to trigger a clot in a capillary, but when I looked I saw that the vessel was already clotted.’”
This was a huge surprise. According to Schaffer, “In the brains of mice, we almost never saw non-flowing blood vessels. Basically all of the capillaries, all of the vessels were always flowing, all the time. That was our impression. And so suddenly, in these Alzheimer’s disease mice, she was finding vessels that weren't flowing and that was super uncommon.”
Her observation triggered them to ask how many vessels were not flowing in the Alzheimer’s disease mice. Schaffer explains, “It took about six months, but then Joan was able to determine that there was about 2 percent of capillaries that weren't flowing in Alzheimer’s disease mice and about a quarter percent that were not flowing in the non-Alzheimer’s, wild-type mice.”
.png)
In short, they had originally received funding to induce blood clots in the brains of Alzheimer’s disease mice and see how that changed the pathology. But they discovered that 2 percent of the capillaries in the brains of these mice were already stalled—something that had not been seen before.
Still, 2 percent of capillaries stalled in Alzheimer’s mice seemed low in comparison to the 30 percent blood flow decrease that they had read about in humans with Alzheimer’s symptoms. It took some vision and further experiments to understand that such a small percentage of stalled capillaries could have a significant impact on the overall cerebral blood flow and even on memory and cognitive function.
What causes the capillary stalls?
Once the team knew that there were more stalled capillaries in Alzheimer’s disease mice, the next question was to determine what caused the stalls.
According to Nishimura, “It could have been small clots, or a constriction in some capillary segments, but it turned out that the stalls were caused by white blood cells that were stuck.”
Blood cells flow single file in capillaries, so a white blood cell sticking in a capillary blocks blood flow and also causes decreased blood flow in other vessels immediately up and downstream. Like humans with Alzheimer’s disease, mice have too much of a small peptide called amyloid beta that can cause inflammation in the brain. In the case of infection or injury, circulating white blood cells stick to inflamed blood vessels and then invade the tissue to help clear the infection and repair the injury.
But it was another unanticipated finding by Schaffer and Nishimura’s team that exposed just how important those stalled capillaries were for overall brain blood flow and, ultimately, for memory function.
The second moment of serendipity
One important research question Schaffer and Nishimura still needed to answer was what kind of white blood cell was causing the stalled capillaries. Knowing the kind of white blood cell could suggest ways to block the adhesion and reduce the capillary stalls. With additional funding from the National Institutes of Health, they divided the work among the people in their lab to discern whether it was macrophages, T cells or neutrophils. To determine what kind of white blood cell it was, they injected fluorescent antibodies into the blood, which would bind to receptors on the surface of cells and help identify their type.
When they injected antibodies to label neutrophils, they used an antibody that bound to the cells’ Ly6G receptor. Again, the team member who made the big discovery was an undergraduate student.
“I can still remember Victorine Muse ’16, M.Eng. ‘17, came in one morning, and she said, ‘Well, I tried the Ly6G experiment, and it didn't work.’ As the head of a lab, I have learned to be very sensitive for certain kinds of words from the team. And one is, ‘It didn't work,’ because that's very ambiguous. What does ‘didn't work’ mean?” recalls Schaffer.
“So we started asking, ‘What do you mean it didn't work?’ She said, ‘Well, when I injected the antibody, none of the stalls were labeled, but they all went away instead.’”
This was incredible news. First, it showed that neutrophils were the culprit, because the protein Ly6G was not strongly expressed anywhere else. But, more importantly, Schaffer explains that, “This finding meant we could use the antibody as a tool to manipulate the stalling phenomena and see what impact that had on blood flow, memory and disease progression.”

In addition to determining the cellular cause of the stalls, this finding opened the door to studies of the consequences of the stalls for Alzheimer’s disease. They had a way to make the blood stalls go away—and a potential window into the forces behind an eventual Alzheimer’s drug target.
Like the earlier stroke of luck where a researcher noticed already plugged vessels when doing an experiment that aimed to produce clots, the discovery that this antibody reduced the stalls came completely out of the blue.
Nishimura notes, “Although antibodies against Ly6G have been used to label neutrophils for decades, this is one of the first physiological consequences that's been described for blocking this receptor, so we were not anticipating this result at all. We were just trying to label the cells, and, to be honest, we really didn’t think neutrophils were a likely culprit. To find that this antibody got rid of the capillary stalls and could be used as a kind of treatment in the mice was a complete surprise.”
Armed with the ability to manipulate the capillary stalls, Schaffer and Nishimura’s team—led by the lead authors Jean Cruz-Hernandez Ph.D. ’17 and postdoctoral fellow Oliver Bracko, and assisted by collaborators from six universities across three countries—launched several studies to explore the importance of these stalls in Alzheimer’s disease.
First, they looked at overall brain blood flow. In their Nature Neuroscience paper, they report that within minutes of administering the Ly6G antibody to the Alzheimer’s disease mice, blood flow in the brain increased by about 30 percent. They also tested the spatial and working memory of the Alzheimer’s disease mice and found that memory function improved within hours of injecting the antibody. This is one of the first treatments described that can improve memory function so rapidly in Alzheimer’s disease mice.
“We do not yet know if this capillary stalling contributes to brain blood flow reductions in Alzheimer’s disease patients, nor do we know if improving brain blood flow will have such a profound impact on memory function,” said Schaffer. “It will take a lot of additional research to lay the foundation necessary to answer those critical questions. The main bottleneck in that research is finding the stalled capillaries, a completely manual data analysis process that is slow, slow, slow.”
The third Eureka moment: solving their data bottleneck with a citizen science game
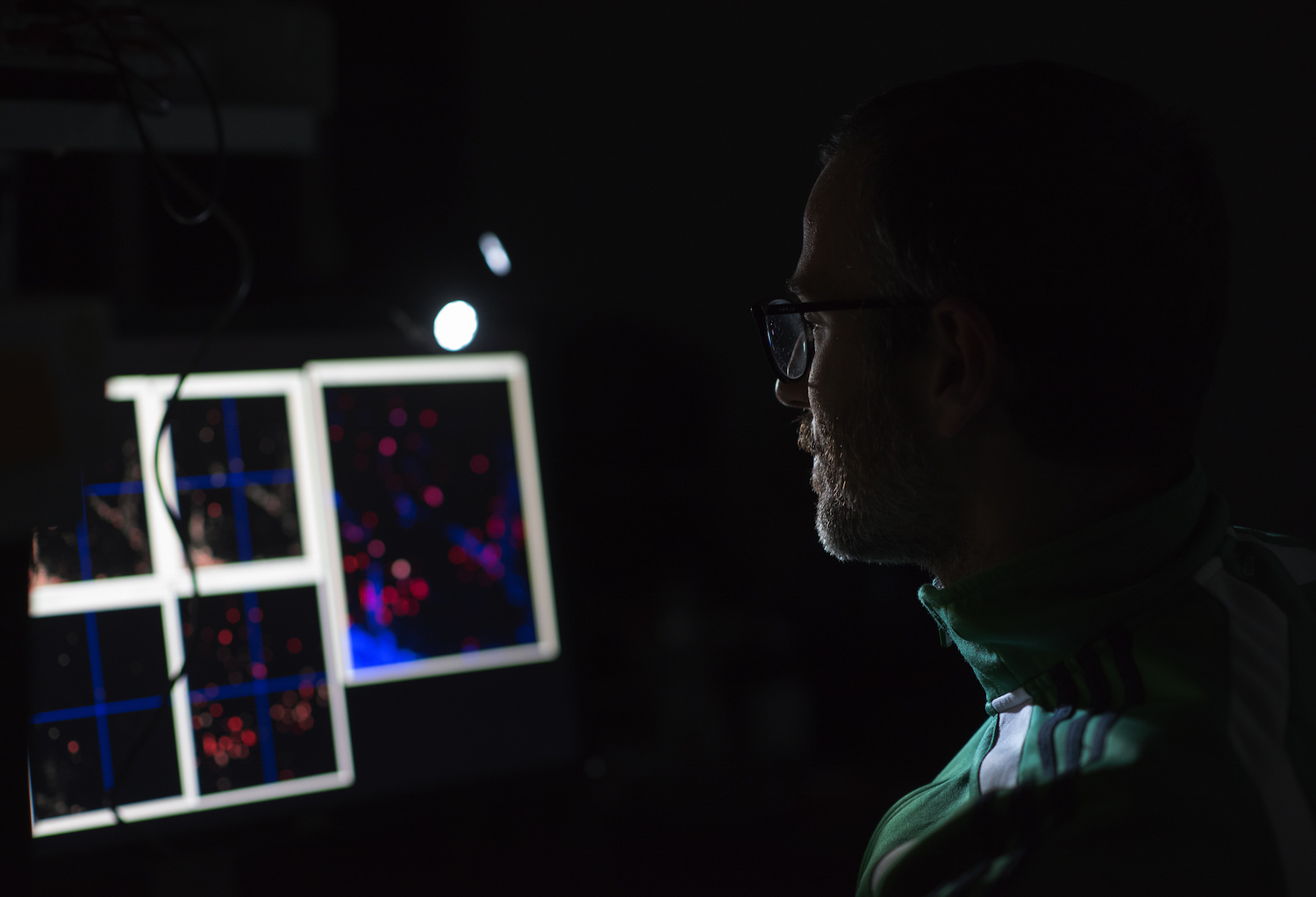
One of the Schaffer-Nishimura Lab’s biggest research challenges is analyzing the image data they take of mouse brains to determine which blood vessels are flowing and which are stalled. The data consists of short videos where blood vessels are highlighted with a fluorescent marker and the red blood cells, which make up about 45 percent of the blood volume, appear as dark shadows inside the vessels. The challenge is to determine whether the red blood cells are moving or not, one vessel at a time.
There would be about four such images per mouse, five mice per group, four to 10 groups per experiment, and dozens of experiments to do. Not only is this a lot of data to keep track of, but it was also difficult for the lab to find any automated methods that could determine whether the capillaries were flowing or stalled. If the lab had to comb through this data manually, it could take decades to move the research forward.
Thankfully, an unexpected artificial intelligence expert helped them figure out a novel way to solve their problem.
In 2013, Janis Dickinson, a professor emerita of natural resources at Cornell who specializes in citizen science, realized that Schaffer and Nishimura could benefit from talking to Pietro Michelucci, the founder of Human Computation Institute. Michelucci, a long-time artificial intelligence expert, understands the capabilities and limitations of this technology. So, he pairs machine intelligence with crowdsourced human intelligence, also know as citizen science, to try to solve big societal problems.
When Michelucci first met Schaffer, he says, “I was a hammer looking for a nail. I had been studying this human-machine partnership for years and had decided it was time to put the science to good use. Schaffer described his promising Alzheimer’s treatment research but explained that the painstaking data analysis would extend their efforts for decades. I asked him to show me exactly what was taking so long. What I saw next gave me chills.”
The blood flows and stalls reminded him of similar images in a famous citizen science project called Stardust@home. Citizen science volunteers, including Michelucci, helped comb through a million images to find star dust particles.
Michelucci contacted the leader of the Stardust@home effort, Andrew Westphal. His father suffered from Alzheimer’s disease, which motivated him to help Michelucci adapt the platform to meet Schaffer’s and Nishimura’s needs.
In 2016, Michelucci and his team, funded by the BrightFocus Foundation, launched the game Stall Catchers, a first of its kind citizen science game that allows anyone to contribute to Alzheimer’s disease research. In the game, participants are shown a movie of blood vessels with a specific capillary highlighted, and are asked whether they see moving red blood cells in that capillary segment. So far, the game has recruited more than 10,000 players.
.jpg)
“The impact Stall Catchers has had on this research is astounding,” said Schaffer., who added that for some of his lab members, one of their primary jobs, for years, was doing capillary scoring. Progress was slow because it could take months to analyze data from an experiment to know what happened and then plan the next experiment. With Stall Catchers, the data analysis can now keep up with the experimental throughput of the lab. Already, Stall Catchers has analyzed data that will, in upcoming papers, answer several important questions, such as how late into disease development can reducing capillary stalls improve brain blood flow and memory function.
Future research directions
Now, the Schaffer-Nishimura team, with the assistance of Stall Catchers, has a number of research pathways they want to pursue. Also with the support of the BrightFocus Foundation, they are testing FDA-approved drugs that prevent neutrophil adhesion and are primarily used to treat autoimmune disease and multiple sclerosis. None of these drugs have been tried in Alzheimer’s disease because there was no reason to think they would help with any symptoms. If any of these drugs works to reduce the capillary stalling in Alzheimer’s disease mice, this could potentially lead to a clinical trials on humans.
Another idea is to find exactly why the neutrophils stick to the walls of capillaries and try to make them not stick without hurting the actual neutrophils, which play an important role in one’s immune system—this is why a drug replicating their neutrophil blocker would probably not be beneficial. They are also potentially interested in examining the retinas of mice and checking for stalling that way, as this may also be possible in humans.
Of course, the road to an Alzheimer’s treatment is a long one, particularly since the lab has only tested their strategies so far on mice. But, if their experience has proven anything, their next breakthrough could depend on the fresh perspective of someone less experienced than them.

